Patient of the Month- Alison S.

If you would like to donate to Soft Bones in honor of Alison, please click the button below!

Hi, I’m Alison, and I’m thankful for the opportunity to share my story of living with hypophosphatasia (HPP).
For many years, I knew something wasn’t right in my body, intuitively believing my body wasn’t metabolizing well. Looking back on my childhood, I displayed symptoms of HPP.
My mom breastfed me till around two years old, yet I was underdeveloped, weighing only 18 lbs at two years old, and missing milestones like standing and walking. With my delayed development, the doctors mentioned ‘failure to thrive’ and originally thought I had a tumor in my pituitary gland, and I underwent testing, but thankfully, it was not the case. During rounds of testing, X-rays of my hands showed my bones were not maturing – calcium was not depositing correctly to mineralize the bones in my hands.
Not long after those tests, my mom stopped breastfeeding me, and I transitioned to eating mostly solid foods. Finally, I began to grow and gain weight. Though I would remain petite, growing only to 5’0 tall, and stay thin in weight. Throughout my childhood, I experienced other health challenges, such as gastrointestinal issues, requiring weekly suppositories until I was 6 years old.


Despite the health challenges in early childhood, I had a lot of energy and was always active, playing with friends, riding bikes, running, swimming, and more. After these activities, I enjoyed recharging my batteries and taking long naps. As I grew older, I loved and valued sleep. I stayed active and energetic as a teenager, playing sports,
hanging out with friends, and participating in various organizations. I was healthy and grateful for those fun, active times in sports and school. In my 20s and early 30s, I chased my dreams, moved to the West Coast, and lived in London. I’m thankful for all the experiences I had during those years.

By my mid-30s, I began to experience health issues like extreme fatigue, brain fog, and painful peripheral neuropathy. I saw several different primary care doctors, and despite out-of-range low alkaline phosphatase (ALP) in my bloodwork, the doctors never said anything and dismissed me time and time again. In 2015, I advocated for my health and pushed to see an endocrinologist, who said she thought I had malabsorption or celiac disease, and sent me to a dietitian. During that time, I made changes to my diet, removing gluten, adding iron, and reducing intake of processed meats and other foods, and began to feel somewhat better, eliminating the neuropathy. I continued to question the low ALP, and the endocrinologist mentioned it could be a rare bone disease, but said she didn’t want to do any further testing, given I wasn’t having any major bone symptoms. I thought changing my diet was all I needed, but years later, I was still fatigued and had low out-of-range ALP on my bloodwork.
In early 2021, during the height of the COVID-19 pandemic, I struggled with brain fog and fatigue again, which made it difficult to focus on work. One day, while spending time with my mom, I was overwhelmed by the sense that something was wrong with my health. Determined to get to the bottom of it, I booked an appointment with a new primary care doctor, a DO. After reviewing my bloodwork and conducting further tests, she immediately referred me to an endocrinologist.

“I think you may have this rare metabolic disease.”
At my first meeting with this endocrinologist, she mentioned my low ALP, and I said, “Yes, I’ve had that low out-of-range ALP value for 7 years now, possibly longer. I just never had access to my medical records before 2014.”
With that, she said, “I think you may have this rare metabolic disease”.
My first thought was no, this cannot be. She told me I would need a B6 blood test, and if it came back elevated, I would likely have this disease. An elevated B6 meant that the B6 was not passing through my blood-brain barrier, which would enable my neurotransmitters to connect properly, hence the brain fog and other neurological symptoms I was experiencing. Sure enough, when my B6 test arrived, it was elevated, and I was shocked. She then sent me for a DEXA bone scan, which showed osteopenia in my left hip.
“Alison, you have hypophosphatasia. It is a rare, multi-systemic disease that is progressive.”
After these further test results, at my next appointment, the endocrinologist said, “Alison, you have hypophosphatasia. It is a rare, multi-systemic disease that is progressive.” Everything she said after that blurred together.
I remember staring at her, trying to process. “This doesn’t make sense,” I said. “Are you sure? Is there anything else we can check?”
The doctor explained, “I’m one of only a few specialists in the U.S. in this disease – your bloodwork and symptoms illustrate the disease, despite you not having all the symptoms, as symptoms can vary widely on a spectrum.”
The endocrinologist began to tell me, “There is an enzyme replacement therapy treatment, but it’s only been tested in children, not in adults. The therapy was approved by the FDA in 2015, and there are risks. But the results have been positive. You will have to do multiple injections weekly. You will likely be on this therapy for the rest of your life, as this is a progressive disease. There’s minimal research, but more is being done yearly as we get more patients on the therapy. As an adult, it’ll be considered an investigational therapy. I’ll leave it to you to make the decision.”
After receiving this news, I got off the phone and cried. After childhood, I had been relatively healthy for many years, ate well, exercised daily, and slept 7+ hours nightly. How could this be happening, especially when I was living a healthier life than most people? I had always been active and fiercely independent. It was hard to accept that I might now have to stop running and doing certain exercises, depend on others to help me with my injections, as well as feel tied to living near good healthcare facilities.
It took me several months to accept the diagnosis. I delayed starting the enzyme replacement therapy (ERT) medication, Strensiq, till I could ask more questions. I’ve been on Strensiq since 2021, and it seems to be helping with fatigue, brain fog, and keeping the osteopenia at bay when taken as directed. The biggest challenge for me is doing the injections. They are painful, and traveling with the medicine, which needs to be refrigerated, can be difficult.


Throughout adulthood, my HPP symptoms have included extreme fatigue, difficulty concentrating, brain fog, neuropathy, muscle weakness, joint pain, and gastrointestinal issues. In recent years, despite exercising nearly every day, I’ve seen and felt a decline in muscle tone and increased joint stiffness. After heavy strength training, my body feels utterly fatigued and in need of a nap to recover.
I was diagnosed with HPP in 2021 at age 42, seven years after bloodwork first showed low ALP levels, and about 40 years after early symptoms like bone issues in my hands and delayed development as a 2-year-old. Between my mid-30s and early 40s, I was dismissed by at least three or more doctors, even though my low ALP levels kept showing up in my test results.

I’m thankful to have found Soft Bones. Over the years, it has been helpful to meet other patients and hear their stories. I am thankful for the advocacy work Soft Bones does in supporting HPP patients in research and treatment, such as organizing the 5-hour FDA Externally-Led Patient-Focused Drug Development, where I had the opportunity to share my patient story with the FDA, clinicians, researchers, and other fellow patients, for future drug development. I’m looking forward to attending my first Soft Bones National Patient Meeting in July.
Being diagnosed with HPP has become a powerful turning point in my life. It motivated me to channel my experience into meaningful work, advising women-led businesses in health and wellness, and collaborating with organizations to develop innovative ventures in health. My journey with chronic illness has inspired a deep commitment to supporting others facing similar challenges, leading me to earn a certification in health and wellness coaching. I am also a member of the Advanced Research Projects Agency for Health (ARPA-H) Investor Catalyst Hub, and recently contributed to an article addressing critical gaps in rare disease research, care, and innovation.
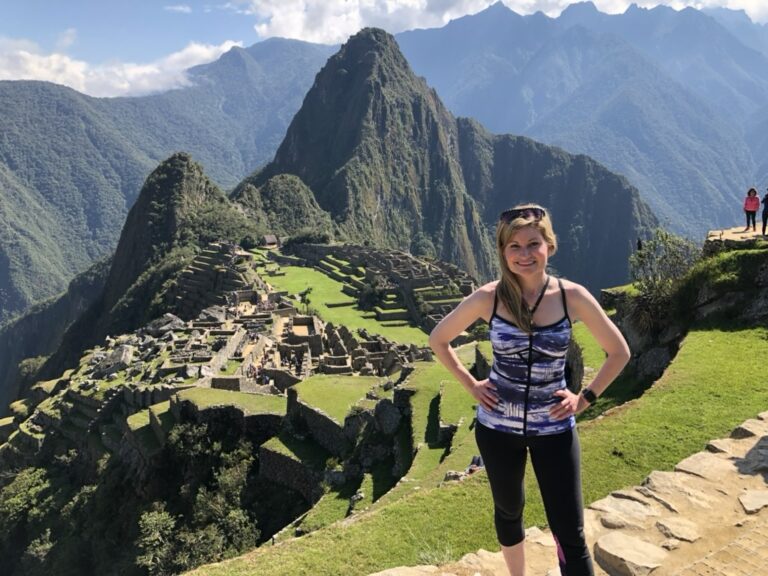
Despite living with HPP, I’m still focused on being active, happy, and living the life I’ve always wanted, such as living by or spending time on the water, traveling internationally, and spending valuable time with family and friends.

To hear from Alison and learn more about her mindfullness tips for Mental Health Awareness Month, tune into Bonafide HPP, Episode 12: A Taste of Mindfulness with Alison S.







Responses