Orthopedic Treatment Considerations for Patients with Hypophosphatasia
Written by Lothar Seefried, M.D.
Head of the Clinical Trial Unit
The Orthopaedic Institute, University of Wuerzburg, Germany
 Diagnosis
Diagnosis
An accurate diagnosis is important for determining the optimal treatment strategy. Because HPP affects every person differently, symptoms and complications from the condition that require medical and/or surgical treatment need to be evaluated on a case-by-case basis. However, some common complications often occur within specific areas of the body. For example, bone-related complications such as fractures, pseudo-fractures, and bone bruises, typically affect the bones of the lower extremities, specifically the femur, tibia, and metatarsal bones. And, bone marrow lesions resulting from injury – or more frequently from repetitive strain in the context of everyday activities – are typically seen in short bones (those that are approximately equal in length, width, and thickness) or in those parts of long bones (those that are longer than they are wide) that are close to the joints.
In contrast, (pseudo-) fractures due to HPP typically occur along the axis (diaphysis) of long bones. Early signs of bone marrow lesions can be detected by magnetic resonance imaging (MRI) before visible damage can be seen on conventional X-ray exams. In case of a suspected diaphyseal (pseudo-) fracture, thorough assessment of conventional x-ray imaging is essential and, in many instances, more meaningful than CT or MRI. Ambiguous findings should be addressed by a bone scan. CT and/or MRI are not mandatory, but may be helpful for specific questions regarding treatment strategy. If a pseudo-fracture is diagnosed, mindful clinical—and in case of doubt, radiographic assessment—is warranted.
Overview:Empty heading
Orthopedic treatment is a critical component of appropriate patient care in hypophosphatasia (HPP ). Important indications comprise correction of skeletal deformities, joint surgery, or treatment of other bone-related complications, specifically fractures and pseudofractures, as well as bone bruising and bone marrow lesions (or bone marrow edemas).
With regards to surgical interventions, the individual patient’s bone quality in the context of HPP, as well as the patient’s personal living situation, specific goals and expectations associated with the treatment should always be taken into consideration.
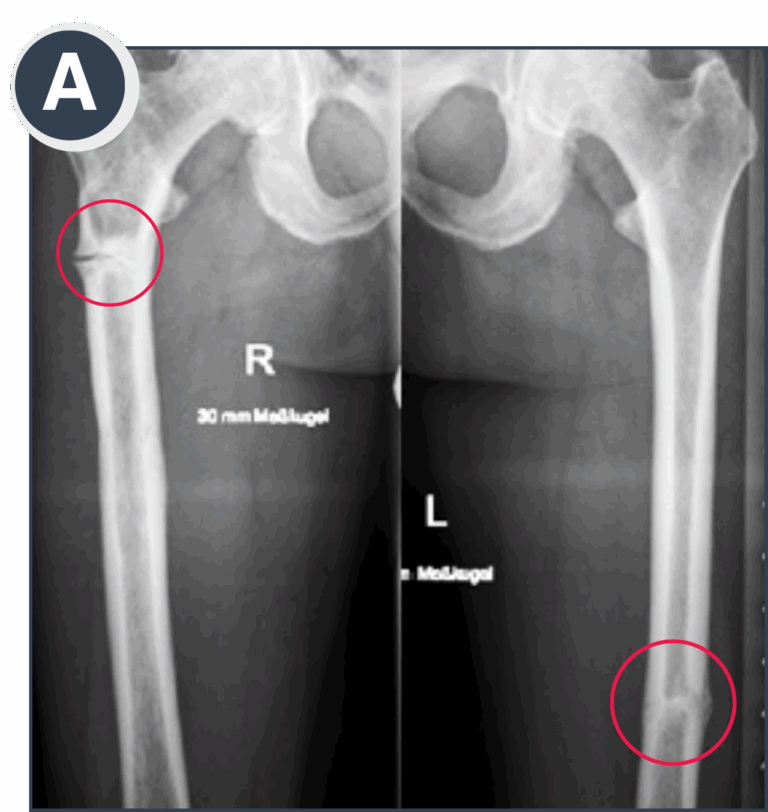
A: Bilateral femoral pseudo-fractures, progressed to almost complete fractures. Symptomatic and painful on the right side, while the left side was asymptomatic and a coincidental finding following thorough skeletal assessment.
 Treatment & Management
Treatment & Management
Non Surgical Treatment:
To compensate for or correct a skeletal irregularity, conservative options, including physiotherapy and braces, should be considered prior to surgery. Particularly with younger patients, medical treatment to compensate for metabolic deficits may also help to correct skeletal irregularities during growth ¹. Early-stage bone marrow lesions should be treated conservatively with suspended weight bearing strictly below the patient’s threshold of pain to allow the bone to heal, and frequently seen concurrent Vitamin D deficiency should also be compensated for mindfully.
Acknowledging that the healing process will take longer for patients with HPP than for those without it, more invasive treatments may not be needed if a patient consequently adheres to this treatment. For pseudo-fractures, suspended weight bearing should be recommended to prevent fracture completion. Although spontaneous bone healing over long periods of time has been seen in some cases and there is some evidence to support treatment with teriparatide, the latter has not been approved for that indication.
Furthermore, despite these treatment considerations, the risk of fracture progression is high. Therefore, in many cases, surgery is advisable to regain mobility and prevent complete fractures or potential deformities. Enzyme replacement therapy (ERT ) has been shown to promote bone healing, even for long-standing pseudofractures, and may even prevent the need for surgery in certain settings ². Currently, the combination of ERT with appropriate surgery appears to offer the best results for patients.
Surgical Treatment:
Surgical treatment for patients with HPP should be performed by a surgeon at a center experienced in both managing and surgically handling patients with HPP or rare bone disorders. If the surgeon is not familiar with HPP, he/she should consult with someone who can share insights from their professional experience.
Pre-surgical planning should assess a patient’s individual situation and determine if the patient’s bones are brittle or soft. X-rays, CT, and MRI can provide some information on the patient’s bone composition, but they do not reliably predict bone quality, so bone density scanning and a comprehensive assessment of bone turnover markers can aid in the understanding of how to best handle the bone intraoperatively. Certain medications, such as enzyme replacement therapy (ERT ) with asfotase alfa, may be initiated prior to surgery and continued through the bone healing process ².
For skeletal irregularities, minimally invasive procedures that will limit soft tissue damage and/or will not require cutting or reshaping of bones should be considered. One such procedure, called (hemi-) epiphysiodesis, typically fuses part of the growth plate of a bone temporarily to delay growth of a long bone. This helps to avoid problems, such as bone fusion failure, during the healing process in corrective osteotomies.
Soft tissue surgery may be needed for some patients, particularly for treatment-resistant situations of heterotopic calcifications at the shoulder, which is the presence of bone in soft tissue where bone does not normally exist. In these cases, minimally invasive arthroscopic (or keyhole) approaches should be considered. These approaches use small incisions and therefore may avoid additional soft tissue damage.
Total joint replacement may be required for some patients, as osteoarthritis is sometimes seen in patients with HPP, even at a young age. These procedures may require special implants to meet the patient’s individual anatomic conditions and bone requirements. Therefore, surgery should be performed at centers appropriately equipped to address potential challenges during the procedures.
For some younger patients, cementless fixation of implants (also called press-fit prosthesis), where the prosthesis is specially textured to allow the bone to grow onto it and adhere to it over time, may even be considered and is feasible in HPP. Other patients may need a cemented prosthesis, which uses fast-drying bone cement to help affix it to the bone.
For other bone-related complications, surgical treatment should rely on well-established procedures that will allow for adequate weight bearing even if the bone doesn’t heal appropriately. In general, intramedullary rodding is considered preferable to plating ³, ⁴.
Using a metal wire, called a cerclage wire, to pressurize or fix the bone is another option, but it has been associated with some healing complications ⁵. Additionally, extensive drilling perpendicular to the longitudinal bone axis should be avoided since healing could be poor and might predispose the patient to additional fractures.
After any kind of surgery, bone healing often takes almost twice as long for patients with HPP as compared to those without it. Ongoing follow-up and monitoring are important for the patient’s long-term treatment and maintenance strategy.
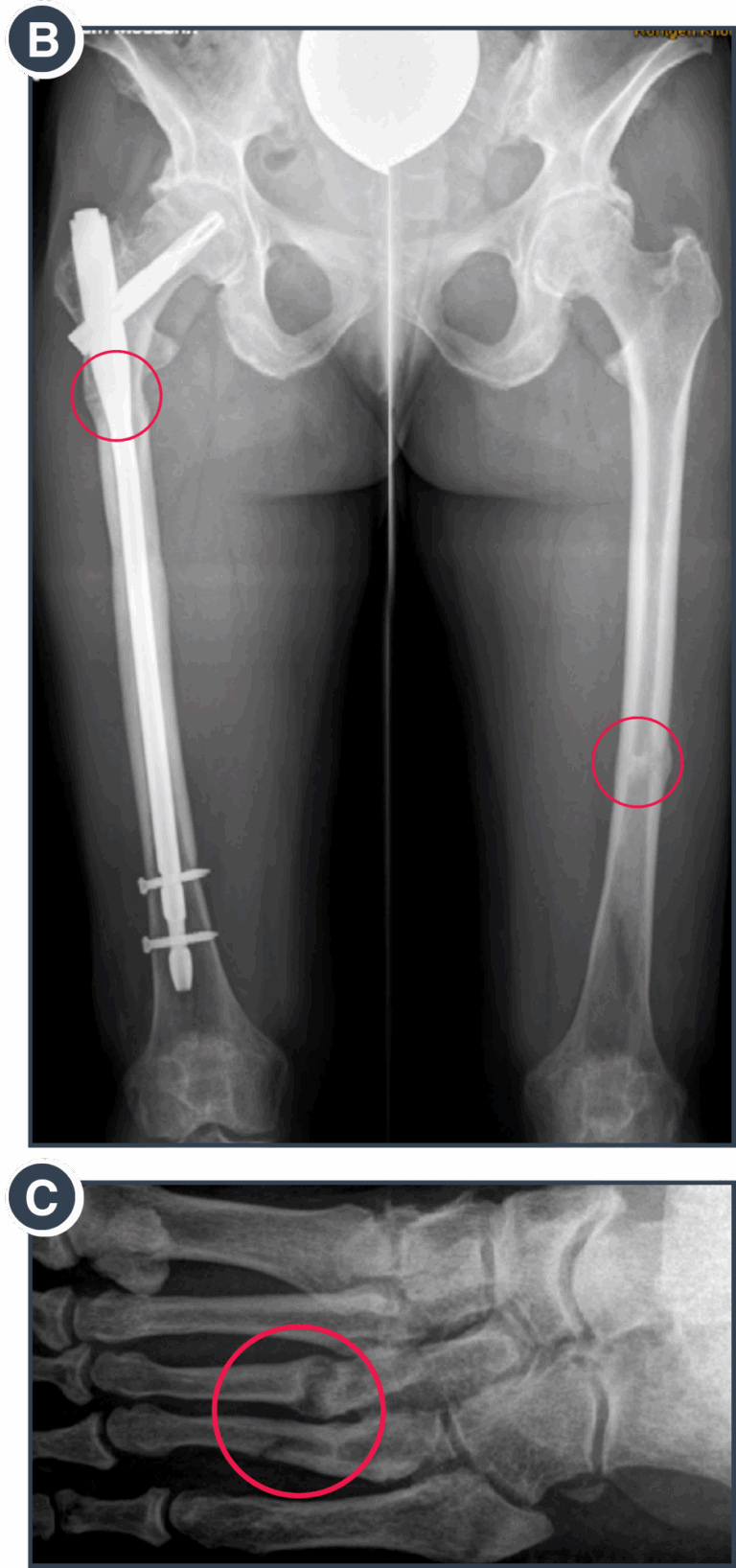
B: Course of fracture healing at 6 months after intramedullary rodding on the more critical right side and initiation of enzyme replacement therapy.
C: Metatarsal fractures due to increased mechanical strain over several weeks in association with enhanced everyday activities.

D: Bone marrow lesion on an MRI in the advanced stage with cortical involvement.
E: Bone marrow lesion in advanced stage with cortical involvement visible on conventional X-ray imaging.
References:
- Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004. 9, Prevention and Treatment for Those Who Have Bone Diseases. Available at https://www.ncbi.nlm.nih.gov/books/ NBK45501/. Accessed October 31, 2019.
- National Organization for Rare Disorders (NORD). Rare Disease Database – Hypophosphatasia. Available at https://rarediseases.org/ rare-diseases/hypophosphatasia/. Accessed October 31, 2019.
- Mao Z, Wang G, Zhang L, et al. Intramedullary nailing versus plating for distal tibia fractures without articular involvement: a meta-analysis. J Orthop Surg Res. 2015;10:95.
- Yu J, Li L, Wang T, et al. Intramedullary nail versus plate treatments for distal tibial fractures: A meta-analysis. Int J Surg. 2015;16A:60-68.
- Agarwala S, Menon A, Chaudhari S. Cerclage Wiring as an Adjunct for the Treatment of Femur Fractures: Series of 11 Cases. J Orthop Case Rep. 2017;7(4):39-43.

