An Introduction to Hypophosphatasia
Michael P. Whyte, M.D.
This publication is distributed by Soft Bones Inc.,The U.S. Hypophosphatasia Foundation
Soft Bones Foundation
was formed in 2009 to provide information and a community to educate, empower and connect patients living with HPP, their families and caregivers. The Foundation also promotes research of this rare bone disease through awareness and fundraising efforts.
Introduction
Hypophosphatasia (HPP) is an inherited disorder that is easy to diagnose if the physician is familiar with the condition. However, most physicians are unaware of HPP, often leading to a frustrating experience for patients and their families
before a correct diagnosis is made. Now, thanks to the internet, physicians and dentists can easily access helpful book chapters and articles published by their colleagues who are knowledgeable about HPP. Unfortunately, not everything on the internet or elsewhere about HPP is accurate or balanced.
HPP has remarkably broad-ranging severity, and therefore assuming similarities from one patient to another may be too reassuring or unduly worrisome.
The biochemical hallmark of HPP is a low blood level of alkaline phosphatase (ALP), typically measured on a routine “profile” or “panel” of blood biochemical tests. ALP is an “enzyme” (a protein that breaks down other chemicals). The resulting build-up of various chemicals in the body due to the ALP deficiency causes the clinical problems of HPP. All physicians expect high ALP levels in the blood when they test a patient with liver disturbances or bone diseases other than HPP, but very few know the causes of a low blood ALP level.
Low ALP in blood serum is expected to be present lifelong for any patient with HPP. Old medical records can be valuable to help determine the patient’s history of ALP levels Nevertheless, low blood ALP levels can also occur in some people who are genetic “carriers” and will not have symptoms of HPP. Importantly, the laboratory that analyzes ALP must provide an accurate age-appropriate normal range for the physician to allow for proper judgment concerning a patient’s serum ALP level. Healthy children naturally have higher serum ALP levels when compared with healthy adults, and therefore a low ALP value in a child with HPP may be misinterpreted as “normal” if the laboratory gives only the normal range for adults in their report.
Furthermore, not everything that causes low serum ALP is HPP. There are other, usually severe, conditions (including some with bone disease) that can also lead to low serum ALP levels. Additional testing, as reviewed below, is necessary to confirm the diagnosis of HPP.
To support a “presumptive” or “working” diagnosis of HPP, physicians in the USA can order a serum level of vitamin B6 (pyridoxal 5′-phosphate), also called PLP, from a commercial laboratory. In HPP, there is a buildup of PLP in the blood because it is not broken down properly due to the low ALP level. PLP is expected to be elevated even in HPP patients who are mildly affected. But, an elevated PLP level can also be found in some healthy “carriers” of HPP. It is important, if possible, that patients avoid taking any supplements containing vitamin B6 for one week before PLP testing in order not to have a “falsely elevated” PLP level caused by the supplements. Testing for an elevated blood or urine level of phosphoethanolamine (PEA), another chemical typically broken down by ALP, is a less sensitive, less precise, and more expensive screening test for HPP, and can be replaced by measuring serum PLP.
The x-ray abnormalities seen in the bones are characteristic of HPP for many patients with the childhood form and the most severe perinatal or infantile forms. Still, these characteristics may not be recognized as diagnostic of HPP even by experienced radiologists. Knowing which x-ray features to look for to help diagnose HPP is of key importance. These features are illustrated in medical books and articles. However, patients with odonto HPP (the common form of HPP that affects only the teeth) do not have bone disease including these x-ray findings.
Accordingly, teamwork is essential to “connect-the-dots” by bringing together a thorough analysis of all of the clinical information (including HPP signs and symptoms, blood study results, and x-ray findings) for diagnosing and classifying HPP patients. In children with HPP, matching “signs” (especially loss of baby teeth before the fifth birthday) and symptoms (sometimes including muscle weakness or bone deformity) is what can lead to the diagnosis. It is important to note, not everything that causes premature loss of baby teeth is HPP. Other disorders can cause this, but in those conditions serum ALP is likely to be normal.
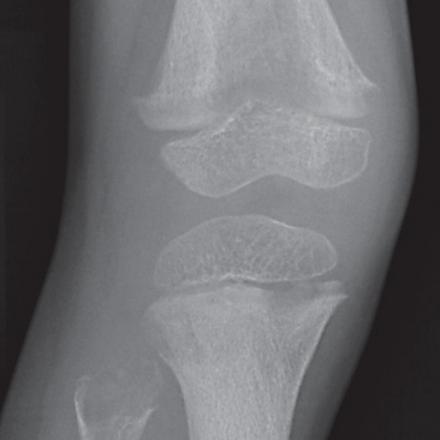
Classic Changes of Childhood HPP
If there is still uncertainty about a diagnosis of HPP, several commercial laboratories in the USA and in Europe offer DNA analysis to look for defects (“mutations”) within the tissue non-specific ALP (TNSALP) gene (the gene is also called ALPL). This gene produces the type of ALP that is deficient in HPP. One or two TNSALP mutations are expected in all HPP patients. Mutation testing can be costly, and is usually unnecessary to diagnose HPP. It is important to note that diagnosing HPP means that signs, symptoms, or complications of HPP are present, and not that a patient has a positive mutation test.
However, mutation testing is necessary to fully understand how the patient inherited their HPP, and therefore if others in the family might also be affected. Mutation analysis is necessary when knowledge about the “recurrence risk” of HPP for future children is requested by the patient or parents. Mutation analysis can help to determine if a spouse is a carrier, or to evaluate the status of a fetus during pregnancy. Mutation analysis can help to identify whether the baby will be unaffected, likely affected, or perhaps a “carrier” of HPP. However, determining which TNSALP mutation(s) is present may not fully predict future clinical problems of tested patients.
Once HPP is diagnosed, further measurements of serum ALP, vitamin B6, etc., are generally not useful. Bone density measured by dual energy x-ray absorptiometry (DEXA or DXA) every few years might provide useful information for adults, but interpretation can be difficult as DXA imaging may not accurately distinguish an increase (“improvement”) in bone density from worsening soft bones (“osteomalacia”). A routine bone scan using a radioactive tracer to survey the entire skeleton can be performed, and followed by x-rays of any abnormal areas identified on the scan. This approach may detect fractures and pseudofractures, particularly in affected adults. Also, evidence for one of the types of arthritis that can affect the joints of HPP patients may be found. Other tests like CT and MRI can be useful to evaluate certain other problems from HPP.
For HPP patients, a primary care physician who becomes knowledgeable about HPP and then helps to coordinate care is important. Medical records must be shared among all involved physicians to optimize their efforts, so it is helpful if patients or parents compile these records and make them available to new caregivers. Treatment at a large medical institution may be necessary, depending on the severity of HPP, and help from the orthopedic surgeon, rehabilitation specialist, pain management specialist, obstetrician, and others can be essential. The medical geneticist can help
to assess the possibility of a future affected child. Pediatric or adult endocrinologists or geneticists, especially those who have an interest in bone diseases, as well as dentists and orthopedists, can help the primary care physician. Good dental care seems especially wise for HPP patients.
 Medical Specialists
Medical Specialists
Although currently few physicians are familiar with HPP, the number of physicians who know about HPP is growing. For the pediatric age group, the medical geneticist or endocrinologist may help confirm the diagnosis, but radiologists and orthopedists may start the search by recognizing (or being puzzled by) the characteristic x-ray
changes (if present) in the skeleton. The pediatric dentist who knows that children should not lose a “baby tooth” before age 5 years, and that normally the root should be absent from the lost tooth, is often the first to suspect HPP during childhood. The pediatrician can become alerted to subtle clinical findings, as can the general internist when HPP first manifests in adult life. Physicians from any medical discipline may then help to diagnose and manage HPP.
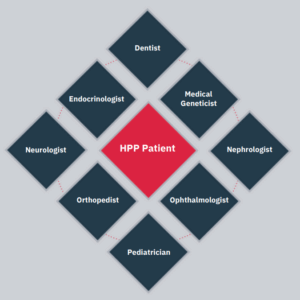
Examples of Medical Specialists
Referrals
Due to an increase in awareness, it is now easier for patients, parents, and caregivers to find physicians who welcome referral of patients with HPP. These physicians may have heard lectures, read about, or perhaps written about HPP. Several patient advocacy groups like Soft Bones, The U.S. Hypophosphatasia Foundation, and others around the world are dedicated to HPP patients, or more inclusively to patients with rare skeletal disorders, and may have a list of physicians who have expressed an interest in treating HPP patients.
Complications
Severely affected infants and young children with HPP may have premature closure of cranial sutures (narrow lines that separate the skull bones and allow the skull to expand as the brain grows). This complication is called craniosynostosis. Craniosynostosis stops one or more parts of the skull from expanding properly in order to accommodate the growing brain. Sometimes in patients with severe HPP, the growing brain is then pushed downward toward the spinal canal by the tight skull. In this circumstance, if there is increased pressure within the brain (often with associated headaches), a plastic tube or “shunt” is placed in the brain, or alternatively surgery is used to reopen the skull for growth.
Orthopaedic surgery may also be necessary, especially in adults, to heal partial or complete fractures or persisting “pseudofractures” in major long bones. Other treatments for HPP may also be necessary for care of the signs, symptoms, and complications, and might include medicines for bone pain or various types of arthritis. Some reports, and our own observations, concerning HPP suggest favorable responses (especially in children) to nonsteroidal anti-inflammatory drugs, but these medicines can hurt the stomach and the kidneys, particularly when used excessively or for prolonged periods, and must therefore be used with caution and only at appropriate doses. Muscle weakness can be a prominent feature of HPP, and occupational and physical therapy may be helpful for treatment of this complication. Dental care is very important for essentially all patients with HPP. In particular, young children with HPP may have difficulties with speech or eating if there is premature loss of many teeth. The help of an experienced dentist should be sought.
Medical Treatment
Sometimes, patients with HPP can have their signs, symptoms, and complications managed by routine medical or surgical means.
For adults with HPP, several physicians have prescribed “off label” the medication teriparatide (Forteo®) given by injection to treat osteoporosis, with some HPP patients benefitting by producing more ALP in their bones. However, teriparatide use is restricted to adults, is not given to children, and is approved to treat osteoporosis for only up to two years.
In 2015, asfotase alfa (StrensiqTM), an enzyme replacement therapy given by subcutaneous injection for HPP, was approved in the U.S., the European Union, and Canada for pediatric-onset HPP, and in Japan for HPP. Detailed information about this significant advance has become widely available.
Patients can also go to www.clinicaltrials.gov on the internet to learn about clinical trials currently underway, and about research opportunities for HPP patients.
*Dr. Whyte has received honoraria and research grant support from, Alexion Pharmaceuticals, Inc., the company that has marketed asfotase alfa for HPP patients.

