What is Alkaline Phosphatase?
Patients with hypophosphatasia (HPP) have a low blood alkaline phosphatase (ALP) level.
ALP is an enzyme (a protein that breaks down chemicals). Most health providers are aware that high ALP levels may indicate medical problems, such as liver disease or other bone diseases besides HPP, but many providers may not recognize that low ALP levels can indicate HPP. Low ALP is important because the inability to break down chemicals can lead to elevated levels of these chemicals, which can cause multiple problems.
The result of low ALP is similar to the result that a vehicular accident has upon traffic; if there is a block in the road due to an accident, then the cars trying to go in that direction cannot move forward and the volume of cars on the road before the accident increases.
Similarly, without ALP, certain chemicals cannot be broken down and instead increase. These chemicals include vitamin B6 (pyridoxal 5′ phosphate, PLP), pyrophosphate (PPi) and phosphoethanolamine (PEA). Elevation of PLP and PPi are thought to cause many of the symptoms of HPP.

 What Lab Tests Are Important?
What Lab Tests Are Important?
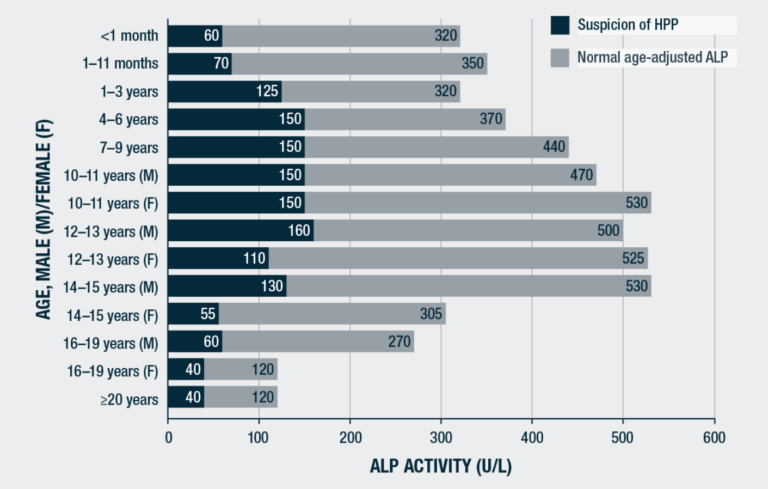
In HPP, blood ALP levels are low. ALP is often measured on routine blood biochemical panels. There are multiple forms of ALP, but the one that is important for HPP is tissue non-specific ALP (TNSALP). This form is measured in these routine panels. Normal blood ALP levels vary between patients based upon age and gender. Children have higher levels than adults, and during childhood, the highest levels occur during infancy and early adolescence. Some labs only report adult normal values
therefore, children who have low ALP levels may be missed, as their levels might appear to be normal using an adult reference range but are actually low for that child’s age. It is important to be certain that a patient’s blood is being sent to a lab that has age and gender-adjusted normal ranges reported.
Once it is certain that an ALP level is low, other tests are typically needed because low ALP levels do not always indicate HPP. In the United States, measurement of the blood level of vitamin B6 (PLP) is generally obtained. In patients with HPP, vitamin B6 (PLP) is elevated. The level of vitamin B6 can be affected by vitamin supplementation with vitamin B6, so it is important to avoid vitamin B6 containing supplements for at least one week prior to measurement. Testing for the other chemicals that are typically broken down by ALP (PPi, PEA) is more expensive and technically difficult as well as less precise, and this testing is therefore not typically performed in the US.
What Happens When PPI &Vitamin B6 Are Elevated in the Blood
In bone tissue, pyrophosphate (PPi) is converted to phosphorus by ALP. Phosphorus then combines with calcium to form mineralized bone tissue. As PPi levels inhibit the formation of bone tissue, an increase in PPi leads to poor bone mineralization, and therefore the abnormal bone findings that occur in patients with HPP. These elevated PPi levels also inhibit the formation of normal cementum, which is necessary to keep teeth attached to the jaw.
On the surface of the brain at the blood/ brain barrier, ALP converts a form of vitamin B6 (pyridoxal 5’ phosphate) to another form of vitamin B6 (pyridoxal) so that it can cross into the brain and help to form neurotransmitters in the brain. Without these neurotransmitters, seizures can occur. These seizures only occur in the infantile form of HPP, and fortunately do not occur in all patients with the infantile form. There is no clear evidence that there are neurologic problems in older patients with HPP
What are the Symptoms of low ALP
Low ALP can lead to multiple symptoms of HPP, including poor bone mineralization and rickets as well as early tooth loss (prior to age 5 years). It is also thought that PPi may build up in muscle tissue and may be responsible for the pain and muscle weakness that some patients with HPP experience.
What should patients ask their doctors about ALP?
It is important to make certain that a patient’s ALP level is being measured by a lab that has age and gender-appropriate normal values.
 What is the treatment for HPP?
What is the treatment for HPP?
In 2015, Strensiq® (asfotase alfa) was approved for use in the US, the European Union, and Canada for pediatric-onset HPP, and in Japan for HPP with onset at any age. The medication is an injection given multiple times per week underneath the skin (subcutaneous). It is a recombinant (factory-made) form of ALP that has a bone-targeting component. When patients take asfotase alfa, ALP levels measured in the blood are quite high (often in the multiple thousands). Therefore, measuring ALP levels is typically not helpful once a patient is on therapy.
Soft Bones: making a difference
As a rare medical condition, HPP presents significant challenges to patients, their families, and caregivers. Finding a physician who can diagnose and treat HPP is often challenging because few doctors have HPP specific training or experience. Soft Bones encourages patients and their doctors to become a team, to address the patient needs and alleviate complications. There is a need to bolster the education and training of HPP in the medical community—and to encourage medical staff to partner with patients in their treatment and care. Patients need more resources and support.
Soft Bones supports research, education, awareness, and policy and patient advocacy. We award research grants to scientists working to understand and treat HPP. We work with the NIH to advocate for government funding for research, and with government agencies to ensure patients receive their entitled benefits. Our role as a sounding board, advocate, and resource to the newly diagnosed patient and caregiver is most important.
This Resource was Written by: Jill Simmons, MD Associate Professor of Pediatrics, Ian Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University Medical Center Director, Program for Pediatric Metabolic Bone Disease

